Why Community Is a Clinical Intervention for Therapists
by Chelsea Fielder-Jenks, LPC-S, CEDS-C, PMH-C
Therapists are trained to notice patterns, attune to nervous systems, and hold space for complexity — but many of us are quietly practicing in isolation.
We sit with clients’ pain, manage risk, document care, and make dozens of emotionally charged decisions every day. Then we often leave our offices and carry all of that alone.
At Healgood, we don’t see that as neutral. We see it as a clinical risk factor — for clinicians and for the people they serve.
Because isolation doesn’t just affect therapists. It affects the quality, ethics, and sustainability of care.
Burnout isn’t just about workload. It’s about being alone with it.
Burnout isn’t a personal failure — it’s what happens when care outpaces support.
You don’t have to do this alone. Healgood Collective is a place for clinicians to be human, together.
Research on clinician well-being is remarkably consistent: burnout is not simply the result of too many clients or too much paperwork. It’s deeply tied to lack of connection, lack of support, and the absence of meaningful professional community.
A review of the mental health self-care literature found that peer support, consultation, and collegial connection are among the strongest protective factors against burnout and emotional exhaustion (Posluns & Gall, 2020). When therapists don’t have places to think out loud, reflect, and be supported by other clinicians, emotional strain accumulates quietly — and often invisibly.
Barlow and Phelan (2007) found that peer collaboration functions as a form of emotional regulation and professional containment, helping counselors metabolize the relational intensity of their work. In other words, talking with other therapists isn’t just helpful — it changes how stress is processed in the nervous system.
Most of us feel this intuitively. When you finally get to say, “This case is hard,” to someone who truly understands, something shifts.
Community is part of ethical practice
Therapists are expected to practice with clarity, attunement, and sound judgment. But those capacities don’t live in a vacuum.
Barnett and Cooper (2009) argue that ethical, effective clinical work depends on what they call a “culture of self-care” — one that includes ongoing peer support, consultation, and professional community. When clinicians are isolated, they are more vulnerable to fatigue, cognitive narrowing, and emotional overload — all of which increase the risk of ethical drift.
Community acts as a form of clinical containment. It gives therapists places to bring uncertainty, countertransference, grief, and doubt. It offers mirrors, perspective, and reality checks. It helps us stay grounded enough to think clearly and respond rather than react.
That’s not indulgent. It’s responsible.
Why Healgood centers connection, not just caseloads
Healgood was built on the belief that clinicians deserve more than office space and scheduling software. We deserve to be known, supported, and in relationship with other thoughtful professionals.
That’s why the Healgood Collective exists — not just as a place to work, but as a place to belong.
We intentionally offer multiple ways to stay connected and resourced, including:
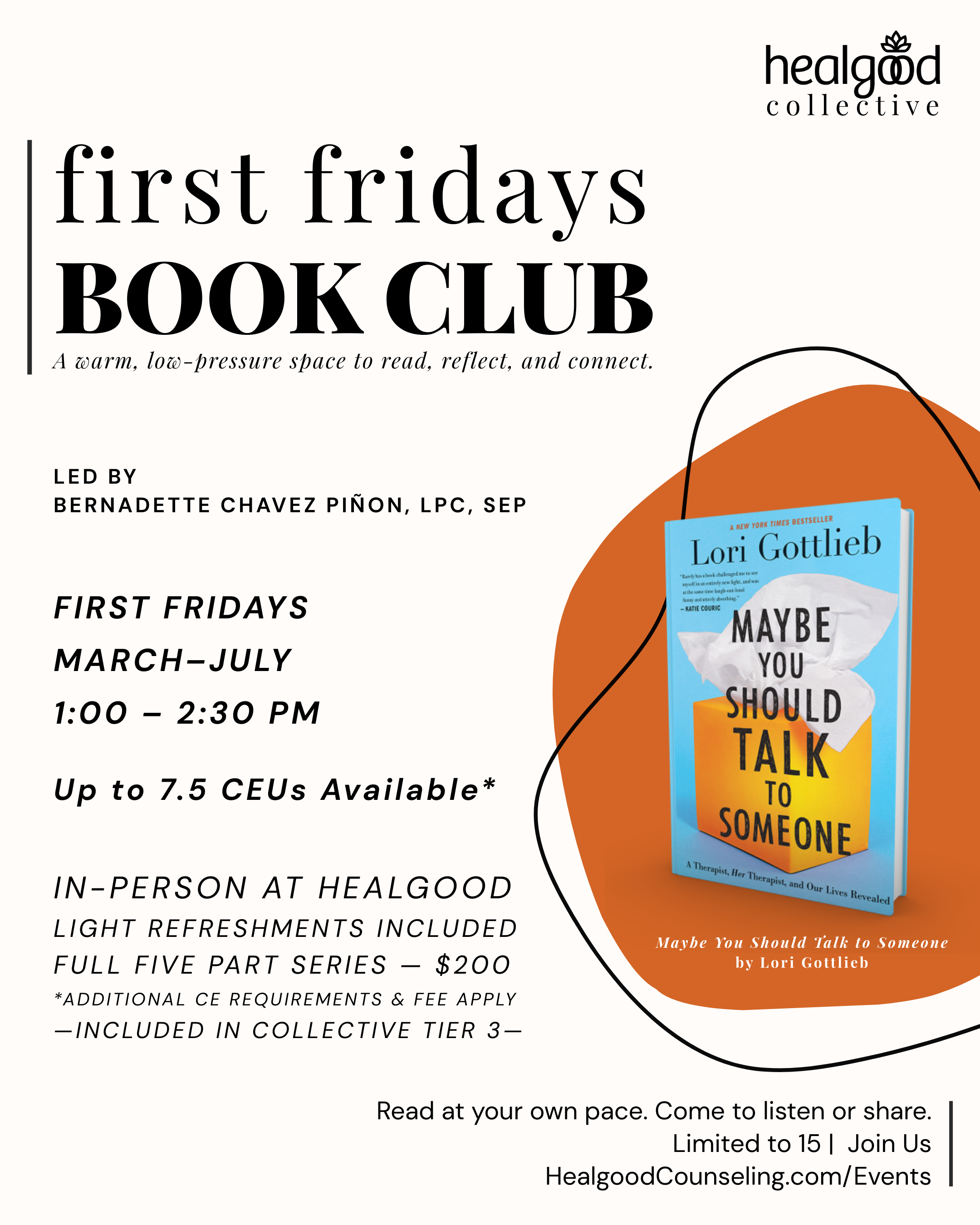
Reflective spaces like our First Fridays Book Club and Monday Mindful Moments
Ongoing consultation groups
Creative, nervous-system-friendly community events
Shared physical space that invites real, human connection
These aren’t add-ons. They’re part of how we support therapists to remain present, ethical, and alive in their work.
The literature backs this up. Therapists who engage in consistent peer support and reflective practice report lower burnout, greater job satisfaction, and a stronger sense of professional identity (Posluns & Gall, 2020; Barlow & Phelan, 2007).
You don’t have to do this alone
Many therapists were taught to be independent, self-sufficient, and quietly resilient. But that model comes at a cost.
Connection doesn’t make you weaker. It makes you steadier.
When clinicians are supported, clients receive better care. When therapists have community, they can keep showing up with curiosity, compassion, and integrity over time.
That’s the heart of what we’re building at Healgood — a practice and a collective that treats community not as a perk, but as a core part of healing.
—Join Us—
References
Barlow, C. A., & Phelan, A. M. (2007). Peer collaboration: A model to support counsellor self-care. Canadian Journal of Counselling, 41(1), 3–15. pdf download
Barnett, J. E., & Cooper, N. (2009). Creating a culture of self-care. Clinical Psychology: Science and Practice, 16(1), 16–20. https://doi.org/10.1111/j.1468-2850.2009.01138.x
Posluns, K., & Gall, T. L. (2020). Dear mental health practitioners, take care of yourselves: A literature review on self-care. International Journal for the Advancement of Counselling, 42(1), 1–20. https://doi.org/10.1007/s10447-019-09382-w